CareXS remote infusion care
Remote infusion administration and monitoring that includes the entire chain of care providers
“How can hospital level of infusion care be brought to the home?”
Project overview
Scope
Client: CareXS
Timeframe: 3 months
Team: UX researcher (Julius), 2 UX designers (including Laurens), product owner, SME, 3 frontend engineers, 2 backend engineer
Methods: field visits & ethnographic interviews, design studio, prototyping, usability testing
Planning
Business problem
An aging population, rising healthcare costs, and a shortage of healthcare personnel result in increased pressure on the healthcare sector. To meet this demand, hospital care needs to be downsized. One solution is to shift care from hospitals to the home in specific healthcare domains. This project aims to investigate if infusion care can be safely provided at home.
Objectives
Understanding of the care processes including all relevant care providers concerning IV infusion administration
Assessment of factors critical to safe home infusion therapy
Designing and testing digital solution that allows for safe infusion administration at home
Research methods

Research
Ethnographic interviews
The aim of the ethnographic interviews with care professionals was 1) to get an understanding of the way care is organized around IV infusion administration across all relevant care providers and 2) an assessment of factors critical for safe at home infusion therapy.
We interviewed 2 home care nurses and 2 hospital nurses as well as the lead hospital pharmacist. All interviews were in person and audio recorded. During the interviews, we asked for protocols, paperwork, and process charts.
We broke down all the steps that IV infusion administration involves across the chain of care providers. We created a service blueprint as well as a happy flow that served as starting point for the information architecture.
As part of the hospital-to-home transition, the specialist, pharmacist, and home care nurse (care team) require to be digitally connected and able to remotely monitor the individual infusion session outside the hospital at the home of the patient.
Several factors were considered critical for safe infusion therapy in the home setting, including appropriate patient selection, assessment and monitoring, and clear communication and collaboration between care providers.
Careful planning and clear communication between care providers during discharge planning is critical as patients are transitioned from acute to home care. Patient and/or caregiver participation in care is a critical aspect of planning.
Service blueprint
Happy flow

Design
Design studio
Having established the care process, the next step was to turn these flows into features and potential UI solutions. We brought together developers, a subject matter expert, and the product manager, and facilitated a design studio workshop. Through brainstorming and prioritizing we explored a set of ideas and moved toward possible design directions.
Wireframing
Having prepared a range of potential design directions, we’ve selected the best ones. Next, we tested our wireframes by interviewing nurses and pharmacists.

Usability testing
Methods
Conducted a usability test with 2 home care nurses, 2 hospital nurses, and 2 hospital pharmacists
All interviews were in person and recorded
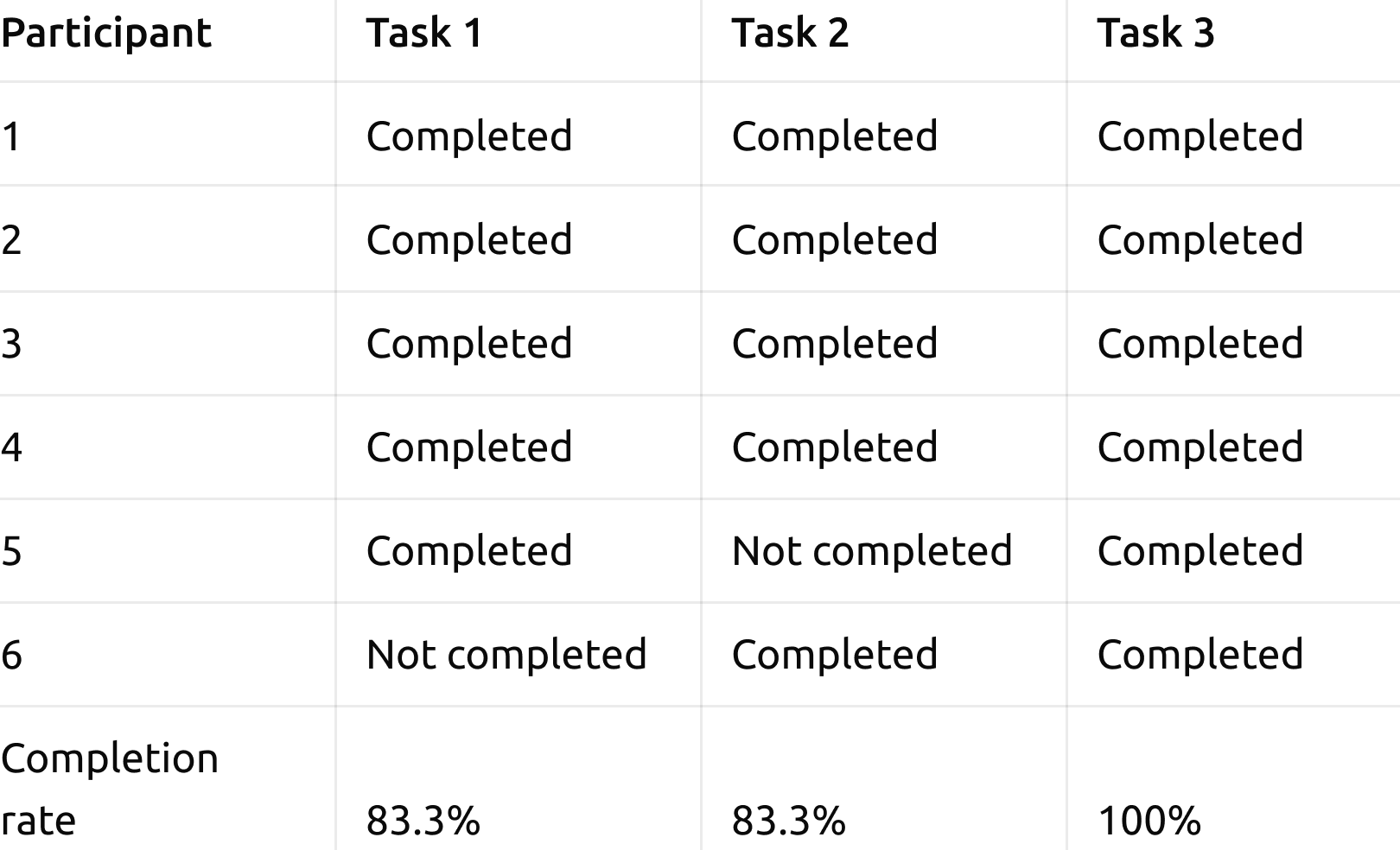
We selected 3 tasks for the users to do during the usability test, including 1) connect a pump, 2) search for a planned infusion, 3) close an infusion
After the completion of the tasks, participants rated the interface on a 5-point Likert Scale with measures ranging from Strongly Disagree to Strongly Agree. Participants also rated the application overall by using the System Usability Scale (SUS) questionnaire.
Findings
Task Completion Rate: 88.6%
Per Task Satisfaction: 4.9
The average SUS score was: 72.3
Users emphasized the benefit of a visual overview to see planned infusions in the region
Users struggled most with the connection wizard for the infusion pump
Metrics
Task completion rates
We measured task completion for each task.
Per Task Satisfaction
For each task, we measured the satisfaction of the user, using the 7-point Likert Scale Single Ease Question (SEQ).
Overall Satisfaction
The user was asked to complete the System Usability Scale (SUS) questionnaire. In that way we were able to better understand the overall system quality

Design improvements
We prioritized usability problems based on the impact of the problem, how many people it affects, and how persistent the problems are. Based on these criteria, two problems were considered critical:
As part of the hospital-to-home transition, the specialist, pharmacist, and home care nurse (care team) needs to be digitally connected to remotely monitor the individual infusion session outside the hospital at the home of the patient. At this moment, different software systems are in use that don’t communicate with each other.
Required activities nurses do when they are double checking injectable medication could be shared with with one colleague at the time. If this colleague isn’t available at that moment to double check procedures, this could result in potential harmful situations.
We created an affinity diagram using the usability data. An important insight became apparent: none of the care professionals wanted to start using another software system. This means that the specialist, pharmacist, and home care nurse need to be digitally connected to remotely monitor the individual infusion session and to exchange information with each other. In order to do so, their current data information systems need to be connected or a new system needs to be put in use. This was an important insight for the development of the company’s business strategy.